Upright Posture Effects
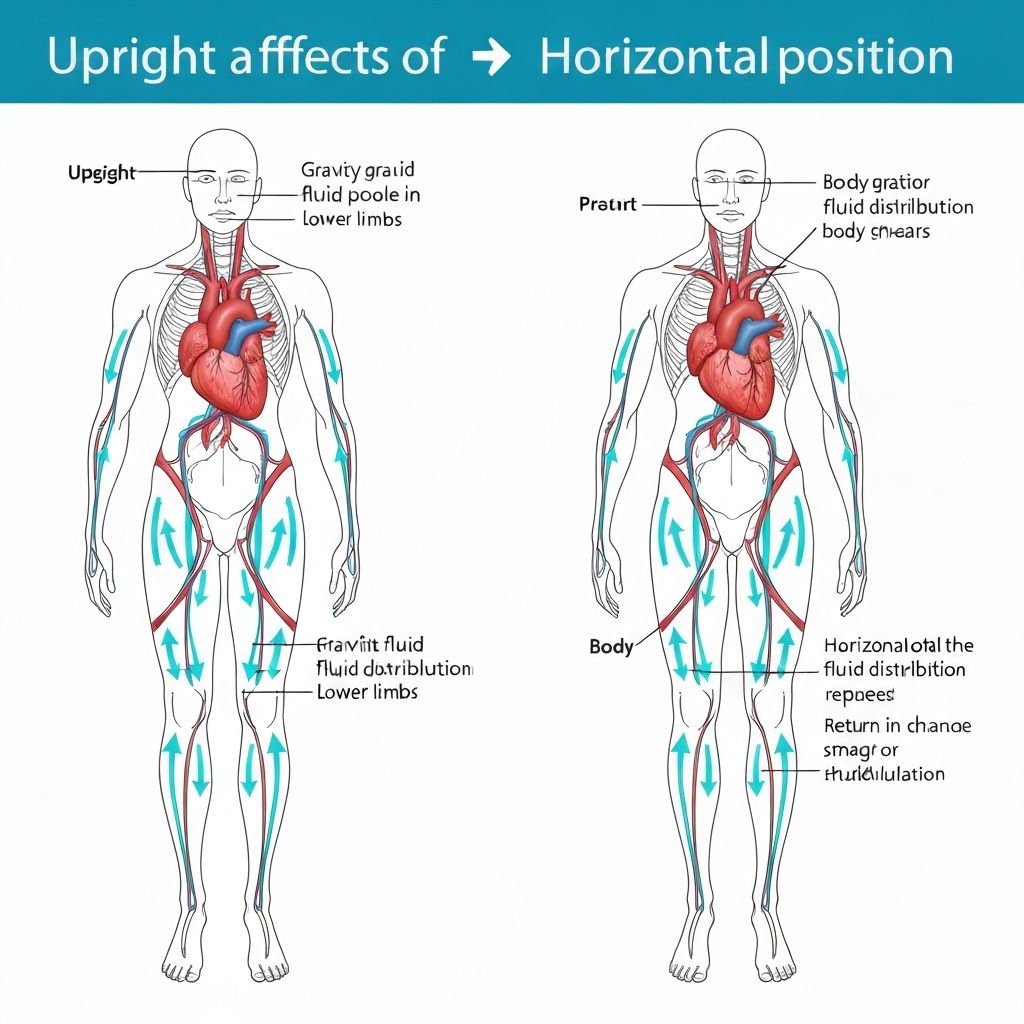
Standing position permits gravity to pull blood and fluid toward the legs and lower abdomen. Approximately 800 mL of blood shifts to the legs during standing. Central blood volume decreases temporarily, triggering baroreceptor reflex responses: increased heart rate, increased cardiac contractility, and sympathetic vasoconstriction in splanchnic and cutaneous vascular beds. These compensatory mechanisms restore cardiac output and central blood pressure.
Abdominal organs and their contents likewise shift downward with standing. Intestinal loops arrange more vertically in standing position compared to recumbent positions. This gravitational repositioning may reduce perceived abdominal distension despite unchanged absolute gas or fluid volumes, as the same volume distributes more linearly along the vertical axis rather than expanding anteroposterior abdominal wall. Individual abdominal wall laxity affects this perception; individuals with greater abdominal compliance may tolerate larger volume changes without pronounced distension sensation.
Recumbent Posture Effects
Lying supine redistributes blood centrally; approximately 800 mL returns to the central circulation. This volume expansion increases central blood pressure and renal perfusion pressure. Enhanced renal perfusion triggers several responses promoting sodium and water reabsorption: decreased renin release reduces angiotensin II production and aldosterone secretion, but simultaneously, atrial natriuretic peptide (ANP) secretion increases from atrial stretch. The net effect typically results in modest urinary sodium and water excretion.
Horizontally recumbent positioning allows abdominal contents to redistribute more widely. Gas and fluid spread laterally and anteroposteriorly, potentially increasing abdominal girth more than identical volumes in standing position. Increased perception of distension in recumbent positions likely reflects this more anterior abdominal wall stretch.